Mitochondrial Encephalomyopathies
Mitochondrial
functions:
cellular energy metabolism
cell
signaling
apoptosis
intermediary
metabolism
metabolism
of AA, lipids, cholesterol, steroids and nucleotides
intracellular
sequestration of calcium
detoxification
of ammonia
Mitochondrial
genetics:
circular
double stranded ring of DNA
2
ribosomal RNAs, 22 transfers RNAs,
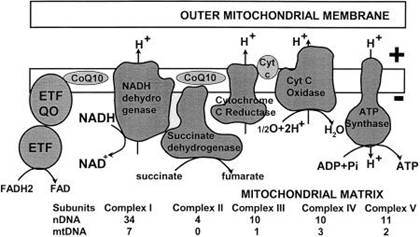
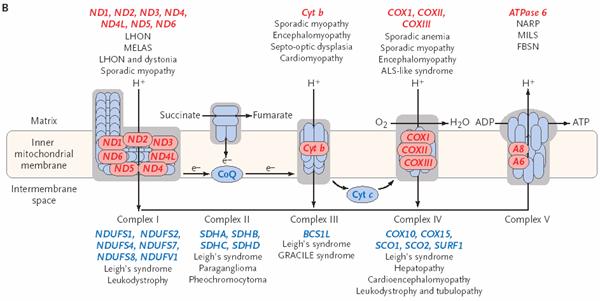
13 polypeptides of complexes I, III, IV, and V of the respiratory chain
2-10 mtDNA rings per mitochondria
cells
contain thousands of mitochondria
Clinical
testing:
resting
serum lactate often elevated due to increase anaerobic metabolism
CPK
muscle involvement
TSH,
glucose, Hgb A1C endocrine dysfunction
serum
AA, urine organic acids, VLCFA, serum biotinidase
metabolic screen
CSF
lactate more sensitive than serum
ECG
cardiac involvement common
EEG
may show slowing
audiography often have impaired hearing
EMG/NCS
help to localize problem to muscle
CT/MRI
often show atrophy and related ventriculomegaly,
white matter changes, calcification (esp brain stem
and BG)
Muscle
Biopsy
H&E, Succinate Dehydrogenase, Modified Gomori-Trichrome,
Cytochrome C Oxidase
Molecular
Studies (Southern Blot, PCR, biochemistry on cultured fibroblasts for
respiratory complex activity)
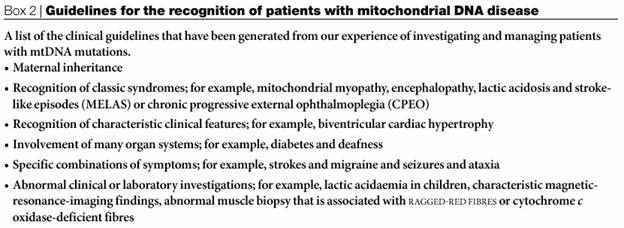
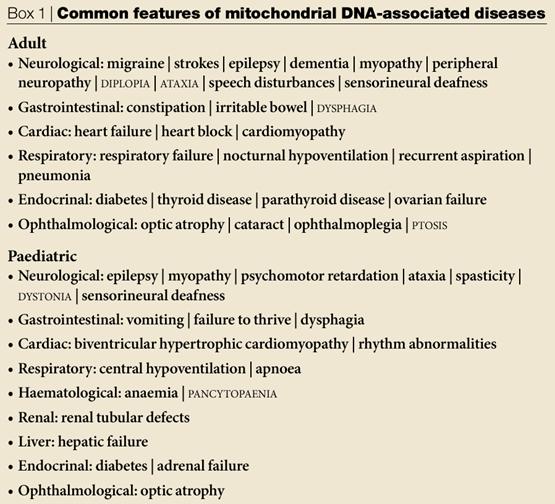
Common mitochondrial
encephalomyopathies:
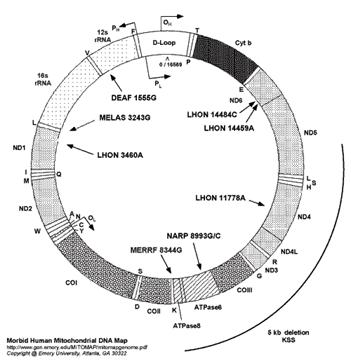
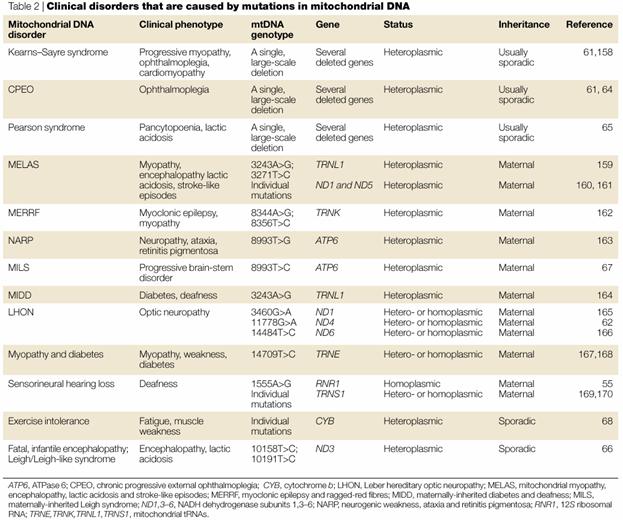
LHON Lebers hereditary
optic neuropathy
- Acute or subacute,
painless, central visual loss in 3rd-4th decade
- Also dystonia
and cardiac conduction defects
- Fundoscopy- peripapillary
telangiectasia, microangiopathy,
pseudoedema, tortuous retinal vessels
MELAS Mitchondrial
encephalopathy with lactic acidosis and stroke-like episodes
- Stroke-like episodes, muscle weakness,
and encephalopathic episodes with high lactate
- Also seizures, dementia, short
stature, migraines, episodic vomiting
MERFF Myoclonic epilepsy
with ragged red fibers
- Progressive myoclonic
epilepsy, action myoclonus, ataxia
- Progressive muscle weakness/atrophy, hypertrophic cardiomyopathy,
dementia, deafness, multiple lipomata
- Ragged red fibers on muscle biopsy
Leigh syndrome
- Not classically one genetic disorder,
but arise from different mutations
- Developmental
delay/regression, central hypoventilation, early hypotonia/late
spasticity
- Optic atrophy, pigment degeneration, nystagmus, ataxia, dystonia,
multifocal myoclonus, seizures
Kearns-Sayre syndrome
- Caused by large deletions in mtDNA
- Progressive external ophthalmoplegia, pigmentary
retinopathy, complete heart block, cerebellar
ataxia, CSF protein > 100 mg/dl
- Progressive external ophthalmoplegia (PEO) can occur independently
Management of
mitochondrial disorders:
- Symptomatic support for seizures,
endocrine abnormalities, etc.
- Unclear role for coenzyme Q10, biotin,
thiamine, vitamins C & K3, carnitine, dichloroacetate
Reference: Taylor RW & Turnbull DM.
(2005). Mitochondrial DNA mutations in human disease. Nature Rev Gen.
6:389-402.